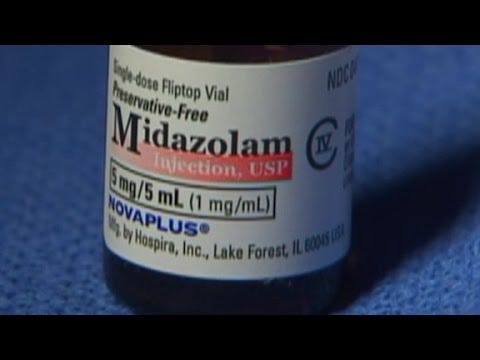
Midazolam in executions.
Midazolam and Fentanyl are known to produce respiratory depression.
Fentanyl and Midazolam induced Respiratory Arrest and Neuromuscular Paralysis during Day Care Surgery
A case report
Rashid M Khan, Naresh Kaul,* and Punnuvella H Neelakanthan
Author information Article notes Copyright and License information Disclaimer
Abstract
We report a 44 year-old, American Society of Anesthesiologist Class I (ASA I), female patient scheduled for elective excision of a small lipoma of the left thigh. She went into a 90 minute apnea and complete muscle paralysis as evidenced by the absence of all stimulatory responses by a peripheral nerve stimulator after receiving midazolam (1.0 mg) and fentanyl (100 μg) intravenously for sedation and analgaesia. The patient made an uneventful recovery after 90 minutes. No cause and effect relationship could be established between the administered drugs and this unusual response.
Keywords: Day case surgery, Midazolam, Fentanyl, Apnea, Muscle paralysis, Case report, Oman
The use of small doses of midazolam and fentanyl is standard practice during day case surgery for providing sedation and analgaesia during minor procedures under local anaesthetic infiltration. Although both midazolam and fentanyl are known to produce respiratory depression in the occasional patient,1 complete apnea with total loss of train-of-four response on peripheral nerve stimulation has, as yet, been unreported. We here report a very unusual case of midazolam and fentanyl induced apnea with total skeletal muscle paralysis in a patient undergoing a small lipoma excision under local anaesthesia.
The counter-indication for Midazolam includes BREATHING DIFFICULTIES.
The presence of other medical problems may affect the use of this medicine. Make sure you tell your doctor if you have any other medical problems, especially:
Alcohol or abuse, or history of or
Drug abuse or dependence, or history of or
Lung or breathing problems or
Muscle or nerve problem (eg, myasthenia gravis)—Midazolam may make these conditions worse.
Glaucoma, narrow-angle—Use is not recommended in patients with this condition.
Heart failure or
Kidney disease or
Liver disease or
Obesity (overweight)—Use with caution. The effects may be increased because of the slower removal of the medicine from the body.
Hypotension (low blood pressure) or
Lung or breathing problems (eg, COPD) , severe or
Patients in shock or with loss of consciousness (coma) or
Sleep apnea (temporary stopping of breathing during sleep)—Use with caution. May increase risk for severe and serious breathing problems (eg, respiratory depression).
This medicine may cause respiratory depression (serious breathing problem that can be life-threatening), especially when used with narcotic pain medicines. Tell your doctor if you are using any narcotic medicine, such as droperidol, fentanyl, meperidine, morphine, or secobarbital.
OK SO LET’S GET THIS STRAIGHT. MIDAZOLAM WITH OPIODS CAUSE BREATHING DEPRESSION THAT CAN BE LIFE THREATENING.
NOW READ THE BELOW MANAGEMENT PROTOCOL FOR END OF LIFE DUE TO COVID - INSANE PROTOCOL REQUIES MIDAZOLAM AND OPIODS. OH. SHIT FUCK DAMN WE WERE KILLING THEM.
“SYMPTOM MANGEMENT FOR SHORTNESS OF BREATH/ANXIETY”
Fact Sheet | Last Updated May 12, 2020 SYMPTOM MANAGEMENT FOR SHORTNESS OF BREATH/ANXIETY|1 of 6
“Symptom management of patients with COVID-19 receiving end-of-life supportive care outside the ICU(1) can be managed by generalist nurses and prescribers. Clinical consultation by the local health authority palliative consult team may be helpful.
Prescriber and nurse utilize a team approach to discuss diagnosis and probable short prognosis with patient and family, ensuring they are aware that medications to manage symptoms may also cause drowsiness.
General information
Dyspnea is the uncomfortable sensation of being short of breath. It may or may not be associated with hypoxia. (3)
Palliative monitoring parameters should be discussed with physician and it is important to assess if symptom relief occurs. Use the Richmond Agitation Sedation Scale (RASS)(6) if using only benzodiazepines, or Pasero Opioid Sedation Scale (POSS)(5) if on opioids and benzodiazepines
Opioids are the mainstay of dyspnea management, however, benzodiazepines are helpful adjuvants.
(1, 3) Commonly used opioids are morphine and HYDROmorphone, as they can be given by subcutaneous route. (1) (avoid codeine)
Midazolam is a short-acting hypnotic-sedative drug with anxiolytic, muscle relaxant, anticonvulsant, sedative, hypnotic, and amnesic properties. (6) It belongs to a class of drugs called benzodiazepines. Rapid onset of effects and short duration of action.(6)
With multiple doses midazolam gains in potency because of a prolonged plasma half-life.(6)
Lorazepam should be tried first as an adjuvant for anxiety, however, for severe anxiety/shortness of breath, midazolam can be used.
(1) In palliative care, medication can be given by subcutaneous route: Insert a Subcutaneous butterfly; use a separate butterfly for each medication. (9)
Continue to treat underlying medical conditions with regular medications (e.g., digoxin for heart failure or inhalers for COPD) as long as possible.
Symptoms relieved by opioids
• Dyspnea(1)
• Cough(1)
• Acute respiratory distress and agitation(1)
• Relief of these symptoms can conserve energy(1)
Symptoms relieved by benzodiazepines
Anxiety(1, 2)”
THIS FACT SHEET SHOULD BE REVIEWED IN DETAIL.
SHOULD THEY MORE PROPERLY SAY; SYMPTOMS RELIEVED BY MIDAZOLAM AND OPIODS ARE BREATHING ABILITY AND LIFE FORCE. A re you ‘palliative’ on covid because of the protocol? Would good doctors please consider that Benzodiazepines and opiods that are given in palliative care MIGHT BE COUNTERINDICATED FOR BREATHING DIFFICULTIES.
UBC, Division of Palliative Care website - links to different health authorities, COVID specific orders, updated daily: https://palliativecare.med.ubc.ca/coronavirus/
One wonders if the above evidence presents a decent shot at a class action suit for families of dead relatives treated on this protocol, by creating a care mechanism that produces and/or exacerbates the very symptoms of the disease.
But don’t say IVERMECTIN.


I'm concerned about this. Have you heard about Laurent Mucchielli? He's a social scientist based in France who has been writing about morality and ethics in the context of the Covid-19 pandemic.
If you are fluent in French, his latest book is "Défendre la démocratie: Une sociologie engagée", he published just a few weeks ago.
You might want want to contact him (he's a nice chap):
Laurent Mucchielli <laurent.mucchielli@protonmail.com> via laurent-mucchielli.org
mucchielli@mmsh.univ-aix.fr
<covid@laurent-mucchielli.org>