HEALTH DATA IS THE TROJAN HORSE FOR COLLECTION AND CONTROL and it is for the Global infrastructure that the WHO intends to rely upon.
There is more than one way to skin a cat
TAKE DOWN THE BEAST.
The WHO is an element of focus as it should be. But there are sub forces in globalist architecture that need to be mapped out. In order for the ultimate power grab to have it’s force and effect the data of individuals have to be mapped out. Why do data centres get the nuclear power and the individuals become relegated to intermittent power? the watching, has become more important then the living. How you watch is through elements of micro data. All of life is being mapped for data centres to evaluate. It is the Tower of Babel. Therefore one method to destroy the Beast is to mandate all actual living requirements receive reliable power prior to the watchers.
The push for health care data is not only national. It is international. And its well documented. In a spiritual way it is the unmaking of what is unique and beautiful in the individual and the making of a series of validities that provide you access or thereby deny it.
Health data for Secondary purposes is one of these elements that will work with the WHO architecture of power. and the systemization of that push for this Health data for secondary purposes will be integral to the success or failure of their plans. Thus you must also watch for this march throughout our system.
The OECD has decided that elements of you- are relevant to GOVERNANCE.
GOVERMENT is being replaced by Governance. From a system that enables active participation by we the people, to a system of utter disconnection from we the people.
Governance requires ultimately that all life be broken into increments of measure and evaluation to provide an access based - or denial based society.
We are live the vestiges of a right based society and we must fortify this to buttress against the concept of governance, and the view of human life as cattle (ultimately an occult view of the world).
. Your data space. The collection of queries, the sum of your indices must be streamlined globally. Why.
so AI can govern;
so algorithms decide your utility in society vis-a-vis a useless eater, or useless breather approach. Of course society is a bit rich of a term for what is envisioned. it is corralling. it is the provisioning and the eliminating of life based on the flick of a switch. It is the return of the Greek notion of gods to control.
in essence it is also the in-humane governing the human. it is the slick and cold wires, and pulses, the electrons that shift the decisions to simplistic equations, which decide one’s movement, participation, and even allocation of goods or services. the QR code you so readily acquiesced to is the god of efficiency, it denies the beauty of life (I believe both in GOD, but also in the 2nd law of thermodynamics) ;
in their system of Governance you become not your God spark but their system of how to query, admit or limit you;
Limit you will include subsistence type limitations such as access to mobility, employment, health care, resources like energy, water and food (which is why the smart meter must be hooked in.
When you read the words “public interest”, or sharing your health data internationally for the public interest and such you should immediately visualize Tedros and Gates. The sharing of your health data including on an international level for ‘public interest’, is the WHO emergency scenario.
Public Interest means denial of privacy and insertion of mandatory intrusion, imposition of their desires based on reliance of the decrees such as ‘ the greater good', ‘your safety’. Public Interest is a box that they stuff all their wants into. they pull it out with a study they have funded, and they impose it with a lawfare they have arranged. Public Interest should be mistrusted ab initio, as it becomes the justification for a whole host of intrusions that view men and women and their children as no better then cattle.
Thus we must, yes defy the aims of the WHO. But my theory is that in order to do so with must truly defy the substructure that enables the WHO to carry out their plan.
Let’s start with the OECD, shall we.
OECD Health Ministers “welcomed the Recommendation of the OECD Council on Health Data Governance at their meeting in Paris on 17 January 2017. The Recommendation lays out the framework conditions to encourage greater availability and processing of health data within countries and across borders for health-related public policy objectives, while ensuring that risks to privacy and security are minimised and appropriately managed.”
“The Recommendation is the product of a multi-stakeholder consultation process. The Recommendation calls upon countries to develop and implement national health data governance frameworks according to twelve high level principles, setting the conditions for greater harmonisation so that more countries are able to benefit from statistical and research uses of data in which there is a public interest, and from international comparisons.”
The next stepping stone was published May 11, 2022 and furthers the above goal.
Health Data Governance for the Digital Age: Implementing the OECD Recommendation on Health Data Governance Available from May 11, 2022
“OECD countries are increasingly concerned with having the right data infrastructure in place for producing health statistics and measuring health care quality and outcomes. This relates to information gathered through registries, administrative data, Electronic Health Records (EHRs), and other sources. It concerns data linkage between settings and levels of care, and mechanisms to generate and use timely, actionable data to support better clinical care and research.
“Interest in strengthening health information systems has grown since the COVID-19 pandemic brought into sharp focus the importance of reliable, up-to-date information for decision making.
“The Recommendation applies to the access to, and the processing of, personal health data for health-related public interest purposes, such as improving health care quality, safety and responsiveness; reducing public health risks; discovering and evaluating new diagnostic tools and treatments to improve health outcomes; managing health care resources efficiently; contributing to the progress of science and medicine; improving public policy planning and evaluation; and improving patients’ participation in and experiences of health care.
“The Recommendation recommends that Adherents establish and implement a national health data governance framework to encourage the availability and use of personal health data to serve health-related public interest purposes while promoting the protection of privacy, personal health data and data security.
“Twelve principles set the parameters to encourage greater cross-country harmonisation among the health data governance frameworks of Adherents so that more countries can use health data for research, statistics and health care quality improvement.
“The Recommendation also recommends that Adherents support trans-border co-operation in the processing of health data for purposes that serve the public interest. It further recommends that Adherents engage with relevant experts and organisations to develop mechanisms that enable the efficient exchange and interoperability of health data.
“Finally, it encourages non-governmental organisations to follow the Recommendation when processing personal health data for health-related purposes that serve the public interest and invites non-Adherents to take account and to adhere to the Recommendation”
“The need for an international standard on health data governance
Health data are necessary to improve the quality, safety and patient-centredness of health care services, to support scientific innovation, the discovery and evaluation of new treatments and to redesign and evaluate new models of health service delivery. The volume of personal health data in electronic form is already very large and is growing with technological progress including electronic health and administrative records; behavioural and environmental monitoring devices and apps; and bio-banking and genomic technologies. The scale, capabilities and methodologies of health data gathering, aggregation and analysis are also radically evolving.
“When personal health data are linked and analysed, an exponential gain in information value can be attained to serve the health related public interest, such as improving diagnosis, particularly for rare diseases; identifying optimal responders to treatment and personalising care for better patient outcomes; detecting unsafe health care practices and treatments; rewarding high quality and efficient health care practices; detecting fraud and waste in the health care system; assessing the long-term effects of medical treatments; and discovering and evaluating new health care treatments and practices. Emerging technologies including Big Data analytics, for example, can utilise enhanced computing power to process broad ranges of data in real time, that, when applied to health can, improve patient-care and further the discovery of disease markers and disease-specific solutions.
“However, often the data are held in silos by the organisations collecting them and there are uncertainties on how the potential benefits of the new analytic techniques can be achieved while ensuring the implementation of existing data protection standards and procedures. A 2013 OECD study showed that many OECD Members lack a co-ordinated public policy framework to guide health data use and sharing practices, so as to protect privacy, enable efficiencies, promote quality and foster innovative research.
“There are benefits and risks from health data processing at both the individual and societal levels. The maintenance of a confidential health care system is fundamental to effective individual care and treatment, and to public health. Appropriate reconciliation of these risks and benefits is necessary to best serve the interests of both individuals and societies.
“In addition, international collaboration is essential to enable countries to safely benefit from health data and to support the production of multi-country statistics, research and other health-related uses of those data that serve the public interest.
“It is against this backdrop that in 2014, the OECD Health Committee and the Committee on Digital Economy Policy agreed to jointly develop an OECD standard to tackle those issues – the Council Recommendation on Health Data Governance.
“Countries are still in the process of implementing the Recommendation
This report presents progress made by countries adhering to the Recommendation in implementing it and reports on its dissemination and continued relevance. It was prepared using three surveys (the 2019/20 Survey of Health Data Use and Governance, the 2021 Survey of Electronic Health Record Systems Development, Use and Governance, and the 2021 Survey of Health data and Governance Changes during the COVID-19 pandemic) as well as the results of several workshops including one on Health Innovation through Fair Information Processing Practices in 2021.
The 2022 Report confirms the continued relevance of the Recommendation, which has proven to be particularly important to address the COVID-19 pandemic. Overall, results indicate that there are many Adherents that are still working toward implementation of the Recommendation.
“Next steps
“Over the next five years, the Health Committee and the Committee on Digital Economy Policy will continue developing tools to support the implementation and dissemination of the Recommendation.
“Findings from this report are contributing to a new OECD Going Digital III horizontal project to support countries in strengthening data governance to support the development of digital societies.
“Future work could focus on three areas that pose challenges for Adherents in implementing the Recommendation:
1) increasing the interoperability of health data and data analytics;
2) achieving greater harmonisation of health data governance frameworks for cross-country collaboration involving the sharing and use of health data; and
3) enhancing the sharing of experiences and best practices in health data security in response to the increasing occurrence of malicious attacks on health data.
“Development of the OECD Recommendation on Health Data Governance
“The work of the OECD to support strengthening health data infrastructure and governance and to protect privacy and data security culminated in the OECD Recommendation on Health Data Governance [OECD/LEGAL/0433] (hereafter, the “Recommendation”), which provides guidance for building national governance frameworks that enable personal health data to be both protected and used towards public policy goals.
“The studies described in the previous section were a catalyst for the development of the Recommendation, which was jointly developed by the Committee on Digital Economy Policy (CDEP) and the Health Committee (HC) with the advice of their respective relevant subsidiary bodies, the former Working Party on Security and Privacy in the Digital Economy (SPDE) (renamed since 2019 as the Working Party on Data Governance and Privacy) and the former Health Care Quality Indicators Expert Group (HCQI).
“The development of the Recommendation also involved the advice of experts in privacy, law, ethics, health, government policy, research, statistics and Information Technology and extensive consultations with civil society (the Civil Society Advisory Committee, CSISAC) and business and industry (Business and Industry Advisory Committee, BIAC). The Recommendation was adopted by the OECD Council on 13 December 2016 [C(2016)176] and that was welcomed by OECD Health Ministers at their meeting in Paris on 17 January 2017 (OECD, 2019[7]; OECD, 2017[8]).
“The Recommendation applies to the access to, and the processing of, personal health data for health-related public interest purposes, such as improving health care quality, safety and responsiveness; reducing public health risks; discovering and evaluating new diagnostic tools and treatments to improve health outcomes; managing health care resources efficiently; contributing to the progress of science and medicine; improving public policy planning and evaluation; and improving patients’ participation in and experiences of health care.
“The Recommendation recommends that Adherents establish and implement a national health data governance framework to encourage the availability and use of personal health data to serve health-related public interest purposes while promoting the protection of privacy, personal health data and data security.
“National health data governance frameworks should provide for:
Engagement and participation of stakeholders in the development of a national health data governance framework;
Co-ordination within government and co-operation among organisations processing personal health data to encourage common data-related policies and standards;
Reviews of the capacity of public sector health data systems to serve and protect public interests;
Clear provision of information to individuals about the processing of their personal health data including notification of any significant data breach or misuse;
The processing of personal health data by informed consent and appropriate alternatives;
The implementation of review and approval procedures to process personal health data for research and other health-related public interest purposes;
Transparency through public information about the purposes for processing of personal health data and approval criteria;
Maximising the development and use of technology for data processing and data protection;
Mechanisms to monitor and evaluate the impact of the national health data governance framework, including health data availability, policies and practices to manage privacy, protection of personal health data and digital security risks;
Training and skills development of personal health data processors;
Implementation of controls and safeguards within organisations processing personal health data including technological, physical and organisational measures designed to protect privacy and digital security; and
Requiring that organisations processing personal health data demonstrate that they meet the expectations set out in the national health data governance framework.
[so this would include in the PROVINCES IN CANADA]
“These 12 principles set the parameters to encourage greater cross-country harmonisation among the health data governance frameworks of Adherents so that more countries can use health data for research, statistics and health care quality improvement.
“The Recommendation also recommends that Adherents support trans-border co-operation in the processing of health data for purposes that serve the public interest. It further recommends that Adherents engage with relevant experts and organisations to develop mechanisms that enable the efficient exchange and interoperability of health data.
Finally, it encourages non-governmental organisations to follow the Recommendation when processing personal health data for health-related purposes that serve the public interest and invites non-Adherents to take account and to adhere to the Recommendation. As of the finalisation of this Report, no Non-Members have adhered to the Recommendation.
The Recommendation instructs the Health Committee, in co-operation with the Committee on Digital Economy Policy, to serve as a forum to exchange information on progress and experiences with respect to the implementation of this Recommendation, and to monitor the implementation of this Recommendation and report to the Council within five years of its adoption. The present Report aims at fulfilling the Council’s instructions.
Methodology
“To monitor the implementation, dissemination and continued relevance of the Recommendation, the Health Care Quality and Outcomes Working Party undertook three surveys: the 2019/20 Survey of Health Data Use and Governance, the 2021 Survey of Electronic Health Record Systems Development, Use and Governance, and the 2021 Survey of Health data and Governance Changes during the COVID-19 pandemic.
“The 2019/20 Survey of Health Data Development, Use and Governance measured elements of national health data governance including the implementation of national health data governance frameworks and related regulations and policies. The survey included a detailed review of data development, quality, accessibility, sharing and data security and privacy protections among the custodians of 13 key national health datasets. HCQO delegates, who are officials of health ministries or national health data authorities, co-ordinated the completion of the questionnaire within each of their respective countries.1 Co-ordination of the completion of the questionnaire was more challenging in countries with decentralised health systems.
“For example, in the United States responses have been provided by various divisions within the Department of Health and Human Services (HHS) and by the National Center for Health Statistics (NCHS) based on their portfolios and may not be reflective of the entirety of health data governance in the United States health system.
“Twenty-two Adherents participated in the 2019-20 survey: Australia, Austria, Belgium, Canada, the Czech Republic, Denmark, Germany, Estonia, Finland, France, Ireland, Israel, Japan, Korea, Latvia, Luxembourg, the Netherlands, Norway, Slovenia, Sweden, the United Kingdom (Scotland) and the United States. In addition, Singapore, which participates in work of the HCQO WP and in the CDEP, responded to this survey even though it is not an Adherent.
“The OECD 2019-20 survey was completed by all respondents before the onset of the COVID-19 pandemic in early 2020. As a consequence of the pandemic, all respondents made improvements in health data to support monitoring and managing COVID-19.
“In July 2021, the OECD conducted a Survey of Health data and Governance Changes during the COVID-19 pandemic. This survey examined the state of health data availability, timeliness, access and sharing and the need for and benefits of improved and harmonised approaches to health data governance that were adopted since March 2020.
HCQO delegates were responsible for co-ordinating the completion of the questionnaire in their respective countries. Twenty-one Adherents responded to this 2021 “COVID-19 Survey” including: Australia, Austria, Belgium, Costa Rica, the Czech Republic, Italy, Japan, Korea, Latvia, Lithuania, Luxembourg, the Netherlands, Norway, Poland, Portugal, Slovenia, Spain, Sweden, Turkey, the United Kingdom, and the United States.
“The OECD also conducted a 2021 Survey of Electronic Health Record System Development, Data Use and Governance in February 2021 (“EHR Survey”). Electronic health record (EHR) systems were surveyed separately because they represent a highly relevant and relatively new source of data on patients’ health care journeys and are often managed by different national ministries or agencies from those responsible for national health data. This 2021 survey followed up on a previous 2016 survey on the same topic and measured the governance of clinical data within EHR systems and the technical and operational readiness to utilise electronic clinical records for statistical and research purposes. HCQO delegates were responsible for co-ordinating the completion of the questionnaire in their respective countries. Respondents to the 2021 EHR survey were officials of health ministries or national authorities responsible for electronic health record systems.
Twenty-six Adherents participated in this 2021 survey: Australia, Belgium, Canada, Costa Rica, the Czech Republic, Denmark, Estonia, Finland, Germany, Hungary, Iceland, Israel, Italy, Japan, Korea, Lithuania, Luxembourg, Mexico, the Netherlands, Norway, Portugal, Slovenia, Sweden, Switzerland, Turkey and the United States. In addition, the Russian Federation, which participates in work of the HCQO WP and CDEP, responded to this survey even though it is not an Adherent.”
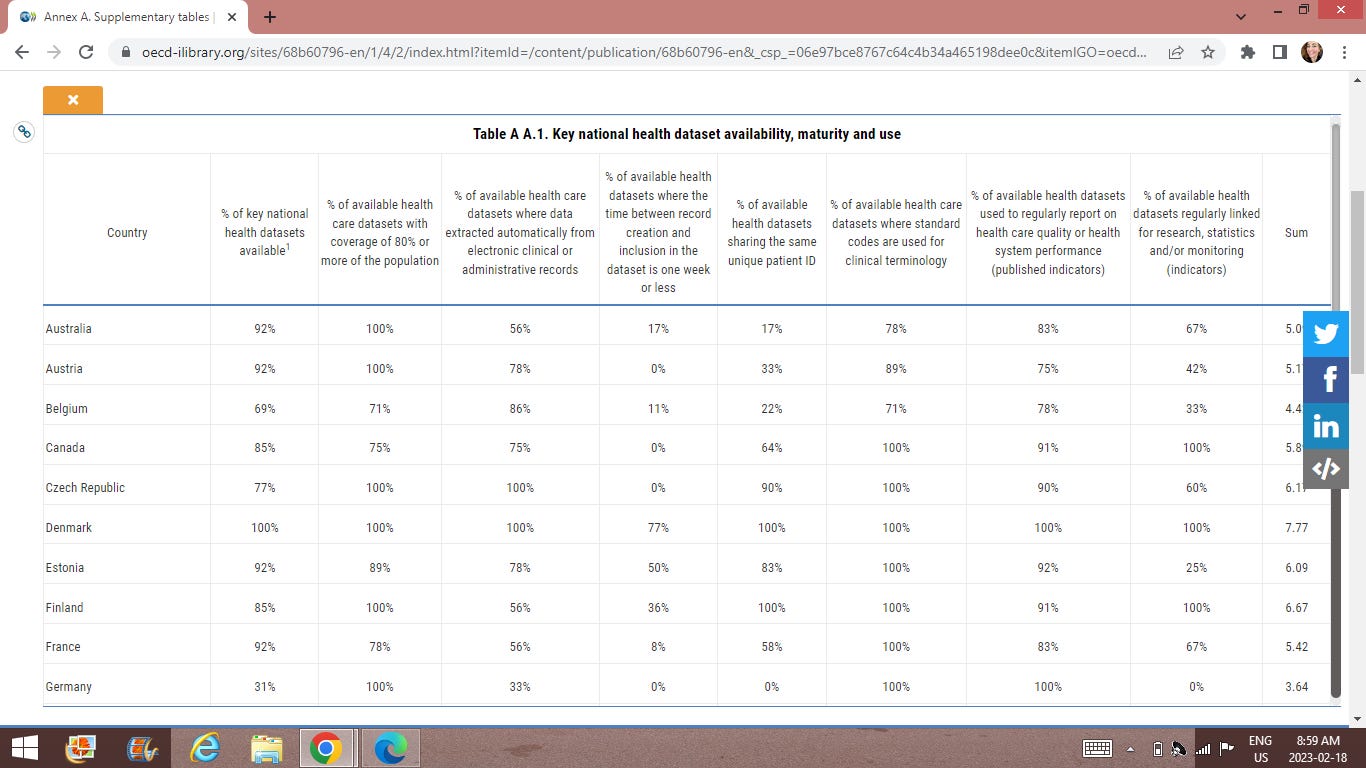
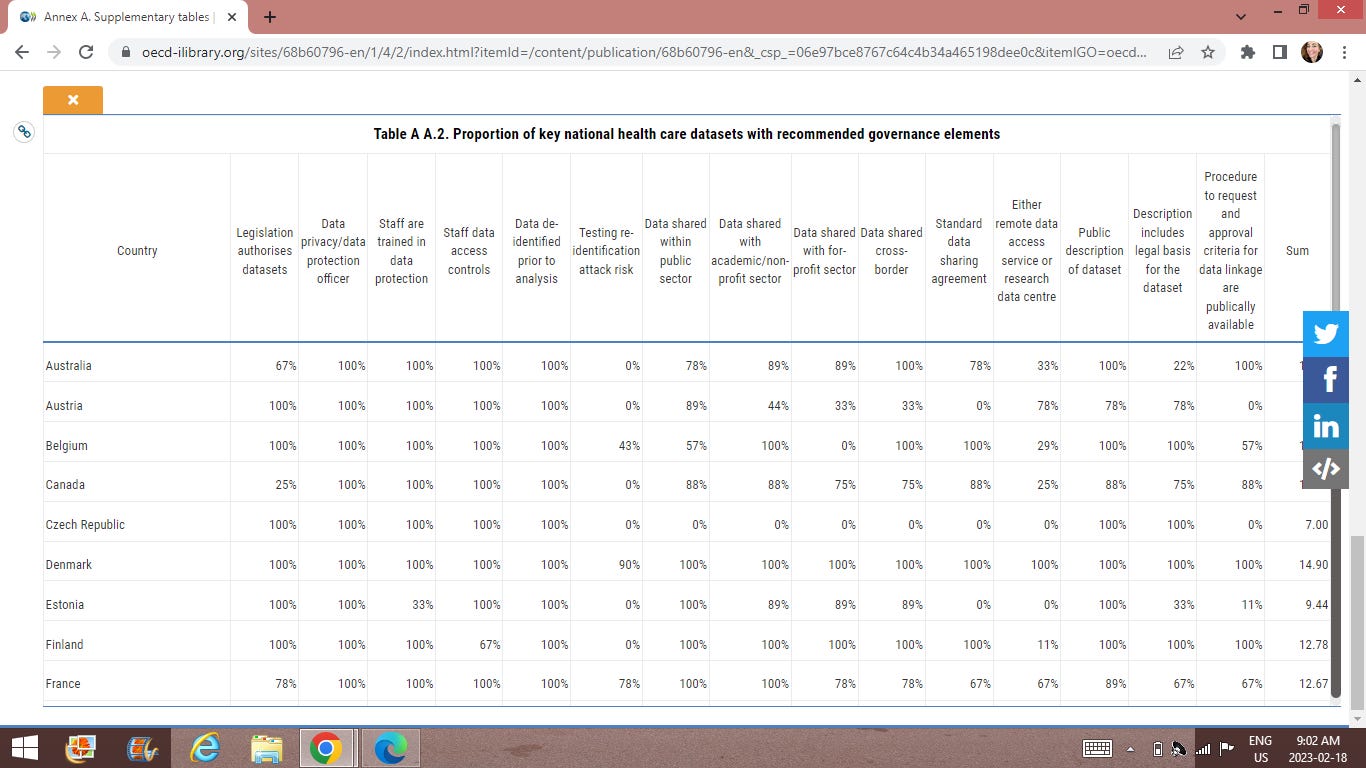
I also found a Table detailing countries progress in this DIGITAL HEALTH DATA PUSH. Note that Canada has very high grades in this area. Isn’t that amazing that no reporter found what I did in response to a reader comment this morning. Please help me out and post all the articles you have on Trudeau’s ‘funding’ for ‘data’ stories.
I will post a follow up Monday based on your help and the other data I found on Canadian Government sites. But this OECD data should slam the tin foil hat article.
But maybe other reporters decided just to look a tiktok and gas light a very serious issue. Do you know your data is being brokered among nations and NGOs? Do your main stream media reporters care? If the image is too small go to the link. Also find your country incase you ARE ALSO BEING GASLIGHT.
Table 1 Key National Health Dataset Availability, Maturity and Use
Table 2 Proportion of Key national Health Care datasets with recommended governance elements
I invite you to go through the entire report. Yes Trudeau wants you Digital Health Care Data. I have found additional national resources to follow. But I want to push this out here because this data set of information can assist people from many OECD nations whos governments are moving to this Agenda without their knowledge or MSM reporting to help them along.
In order to defy the WHO it is not merely their treaty or their INternational Health regulations we must defy. We must defy the the pillars that enable their hegemony.
What is the remedy?
privacy;
national push back on the sharing of data (utilize provincial jurisdiction where possible) Please consider that all changes to the Constitutions will in fact be in order to permit their PUBLIC INTEREST (aka demonic centralized control plans) goals. ;
push back the centralization of data;
require data to be at the patient and doctor level where it belongs;
repeal the legislations passing that provide this data to third parties;
reverse the trend of data collection and measurement;
reverse the ability of data centers to parse it for algorithms;
repeal all laws set out by the OECD as necessary. They are laws for the sole purpose (explain otherwise if it our contention I am wrong so I can make the necessary retraction for your caveat) of enabling a globalist transhuman system of power and control that nullifies the nation state and the protections found with them.
understand that the left that hides and pushes the power through. But if the right is to succeed in pushing back, it will need the list of laws required by the OECD to pass: in order to reverse them. The laws and regulations are the key. These are being hidden in spending omnibus bills in the US. In Ontario Canada Bill 100 hides the ability to take away one’s house and car for protesting. This is something that also must be repealed, along with the strong mayors act, which enables the c40 smart city architecture rolling out in the cities to be bulldozed through. The Human Rights architecture that weaponizes speech must be eliminated in deference to constitutional rights. the Professional Bodies are systems of capture and control through speech committees and must also be reformed.
TAKE DOWN THE BEAST.





Consider the following scenario ...
.
Someone gains illegal access to that Health Data. After a quick browse they notice that the Daughter of the Premier of the Province has been issued Medication that is used exclusively to treat SYPHILIS.
.
PREMIER: "Gee I'm sorry Jane, I did not intend for that to happen".
.
JANE: "That is OK Dad ... ACCIDENTS DO HAPPEN".
.
Like this data..... Nova Scotia is preparing to pass a law to give the government access to all your health information
https://rumble.com/v4ljdq8-nova-scotia-is-preparing-to-pass-a-law-to-give-the-government-access-to-all.html